I ended the previous blog post retelling about the moment Brent, while still ventilated, opened his eyes and looked at me.
The following begins the next day.
FRIDAY
I woke up that morning, got ready and headed to the hospital.
I sent a note to my father-in-law and told him I was on the way.
He informed me that when Brent woke up, he became anxious upon noticing I wasn’t in the room.
When my father-in-law relayed that I was on the way, Brent audibly sighed and relaxed.
I finally arrived with Sprite in tow.
She had yet to see him since his ventilation.
I felt seeing her daddy in that state would be traumatizing.
-Since we’re on the topic of Sprite and I’m remembering as I write, I am reminded of the many people who helped me with childcare and things for her to do during these long days at the hospital.-
-Each and every one of you were a huge blessing to us.-
While Sprite was hanging in the hospital waiting room with family and friends, I visited with Brent, who was still ventilated, though awake and responsive.
I walked in and rubbed his arm.
He looked up at me and smiled, but it was a “I want to hold you, but I can’t” smile.
It was bittersweet.
I kept thinking, “I want to talk with you and be with you, yet I can’t.”
But, those aren’t thoughts you share in those moments.
I also kept wondering, how is he on the inside?
Does he feel trapped? mad? sad? anxious? confused?
It really bothered me that I couldn’t talk with him about what was happening.
He was here right in front of me, and yet, not really.
I missed him.
As these thoughts swarmed my brain, I remembered today was another surgery to check for progress, etc.
Although he had a good couple of days, the surgeon still noticed some spreading redness up his back, so some additional incisions were necessary.
I was really hoping his report would include vent removal, but in addition to the spreading infection, Brent’s lungs were also collecting some fluid.
And, remaining on the vent would allow for easier fluid removal.
I held it together until the surgeon left.
Upon her leaving, I cried.
These weren’t the words I wanted to hear.
I wanted to speak with my husband.
I wanted a sense of returning to normal.
Sprite witnessed my tears and began to cry as well.
I wiped her tears and explained that I was just sad.
She looked at me and said, “I don’t like you sad.”
I snuggled her in close and we cried together.
Soon after this update, he was taken up to his room where shortly after a multitude of visitors came trickling in.
So many people came to his room, inquired about his well being and mine, brought food, offered prayers with and over us.
That afternoon I called Brent’s work and began the process of applying for short term disability.
I could tell he wasn’t returning to work anytime soon, so I made the call.
After I was transferred from person to person, I finally landed an individual who knew what I needed.
I told the lady I needed to begin this paperwork process, but because it was for my spouse, they wouldn’t let me – Brent had to do it.
So, I’m sitting there in the waiting room trying to not completely lose my mind as I’m being told that my husband, who is ventilated, has to provide consent.
I could feel my blood pressure rise and frustration boil to the surface.
With extra shrill and exasperation in my tone I replied, “My husband can’t talk to you because he’s on a ventilator!”
The silence and misunderstanding were palpable.
She may have missed the imbedded message before, but now she understood.
With her revelation, we moved forward with the short term disability process with intent for him to sign and approve once he improved.
As the evening came to a close, his temperature finally fell below 100 degrees.
And, this being Friday night, I jokingly sent a text message to our Kids Director at our church, where we coordinate on Sunday mornings, “I assume there isn’t anything for us to do for Sunday with Sojourn Kids?”
She replied, “Haha, thanks for that. I needed a good laugh.”
SATURDAY
I arrived that morning and had the opportunity to relax with Brent in his room.
He was able to communicate with me through facial expressions and head nods; not ideal, but much better than nothing.
This mode of communication was frustrating because he wasn’t able to use his hands.
They were in restraints.
Although decreasing his sedative allowed for increased responsiveness, it also allows for additional movement without complete understanding.
Many individuals in this position tend to manually remove their vent tubing, so hand restraints were necessary.
Later that afternoon, we had a visit from our pastor and his oldest son.
He checked in on his progress, our needs, and prayed over us.
I, however, made the mistake of waking Brent.
He woke up and saw our pastor, which created some excitement.
But, with the medication fueling some disorientation, the tubing, restraints, and more, he wasn’t able to properly interact or communicate well.
So, this caused a decent amount of frustration for him and total confusion for the rest of us.
After our Pastor left, I continued to try and figure out what Brent was trying to communicate, but to no avail.
Eventually, he just gave up.
He was so frustrated, and I felt entirely helpless.
I really wanted to help him, but couldn’t.
Thankfully, following that episode, we had additional visitors which helped improve his demeanor.
Brent wrapped up the evening with receeding redness and less firmness, as noted by the nurse, and a temperature below 99 degrees.
I saw many signs of healing.
I felt it was an answer to all the prayers being lifted on our behalf.
I wrote in my journal, “God is good, even during trials.”
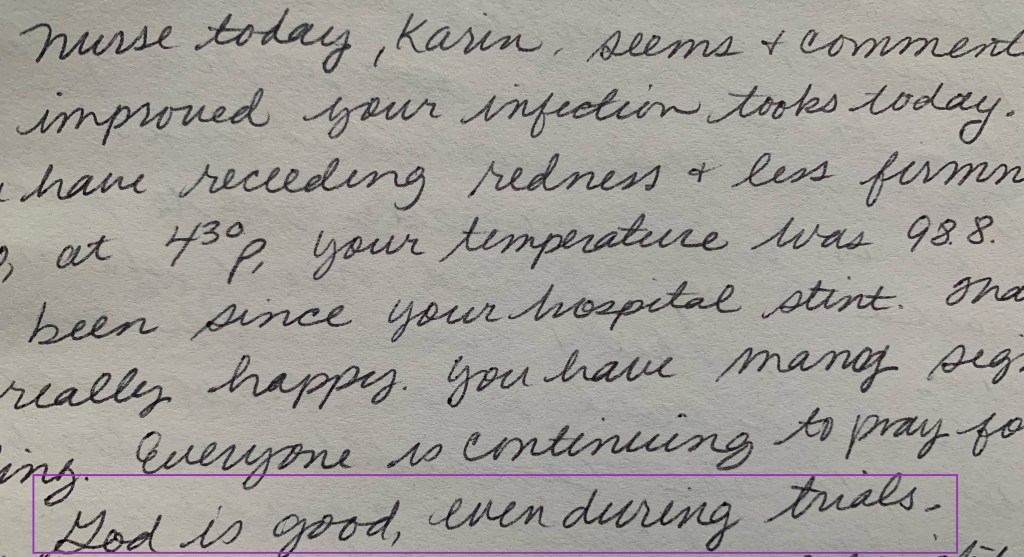
We were far from over, but resting in this promise.
SUNDAY
Before I even arrived at the hospital on this day, I received a text message from my brother-in-law that Brent’s temperature was 97.9 degrees.
The absolute lowest it has ever been since we arrived at the hospital just over a week ago.
As I arrived, I was informed he sported a significant rash on the underside of his body.
His back, back of the arms, and back of his legs were purple from an allergic rash to the penicillin.
We all hoped he would avoid a reaction, but were so glad it took a few days before his body reacted.
To counteract the rash, he was given significant doses of benadryl.
Following this, his nurse gave a heads up that her and some other nurses would be coming in to change his wound dressings.
I couldn’t stay and look.
I’m not normally totally grossed out by things like that, but the dynamics are different when it’s your spouse with the wounds.
Large, open, debrieding wounds at that.
Those of you who don’t know about debridement – it’s where a wound is opened up and the infection drains and airs out.
It’s as horrible as it sounds.
Brent was literally laying in the hospital bed with open wounds, slightly covered to keep some germs out, but, that was it.
While the dressing was being changed, the weekend doctor was making rounds and checked on his progress.
His report would decide if he needed surgery before Monday.
I was in the room, but on the opposite side of the room away from wound view.
I didn’t even write this part in the journal, but remembered upon reading and recollecting that I could see a reflection of the wound in my father-in-laws glasses.
All I could see was a bright white light and red.
Later my father-in-law said it was a good thing I didn’t look because it was bad.
That made my heart hurt.
That his wounds were that shocking and awful.
Thankfully, he received gold stars for his progress.
The doctor noted that he was showing no signs of redness, nor signs of additional necrosis.
So, no surgery needed today, and more than likely not tomorrow, if progress continued.
I remembered posting this updated information on Facebook and was overwhelmed by all the people following his progress.
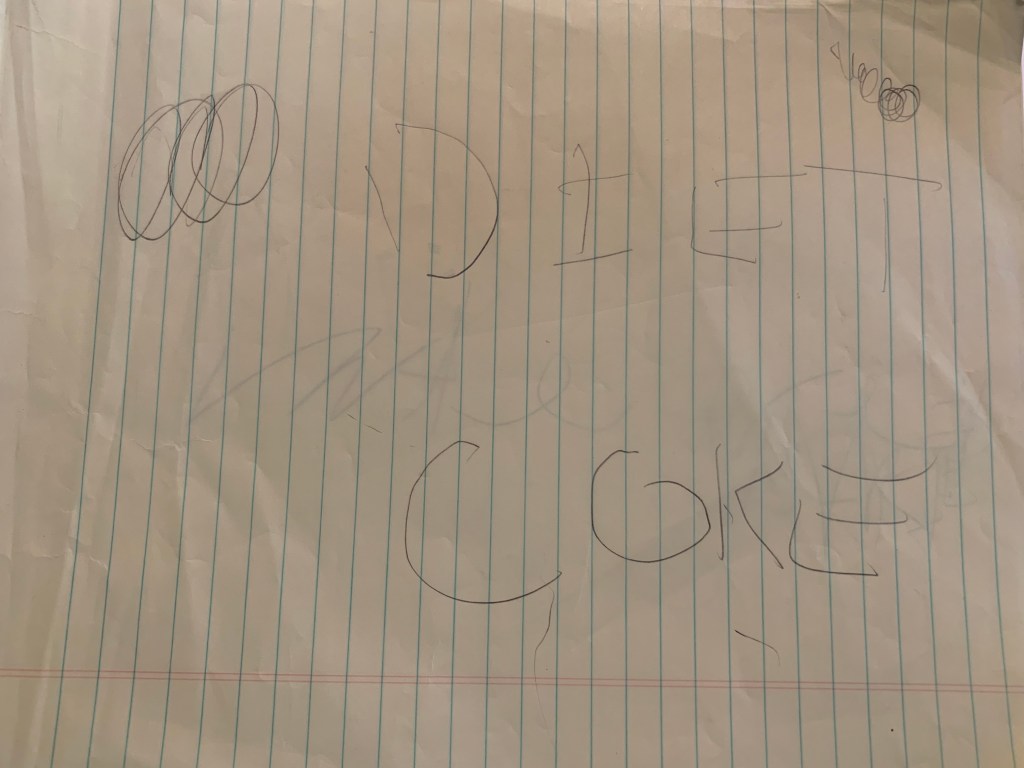
Also on this day, his dad brought pens and legal pads for Brent to use.
As soon as he had the items in hand, he wrote down, “diet coke.”
Soon after that, there was discussion in his room about needing restaurant suggestions.
So, he pulled out his pen and wrote down, “wild eggs.”
His Aunt Janet said, “even while sedated, he’s still the smartest person in the room.”
A very accurate statement indeed.
Later that day, we had a visit from our Kids Director.
She wanted to check in on us.
Just a few days prior she lost her grandfather, and because Brent is so selfless, instead of using the visit to “talk” about himself, he instead asked about her grandfather.
As she was asking questions about his well-being, he pulled out his pad of paper, and wrote the following:
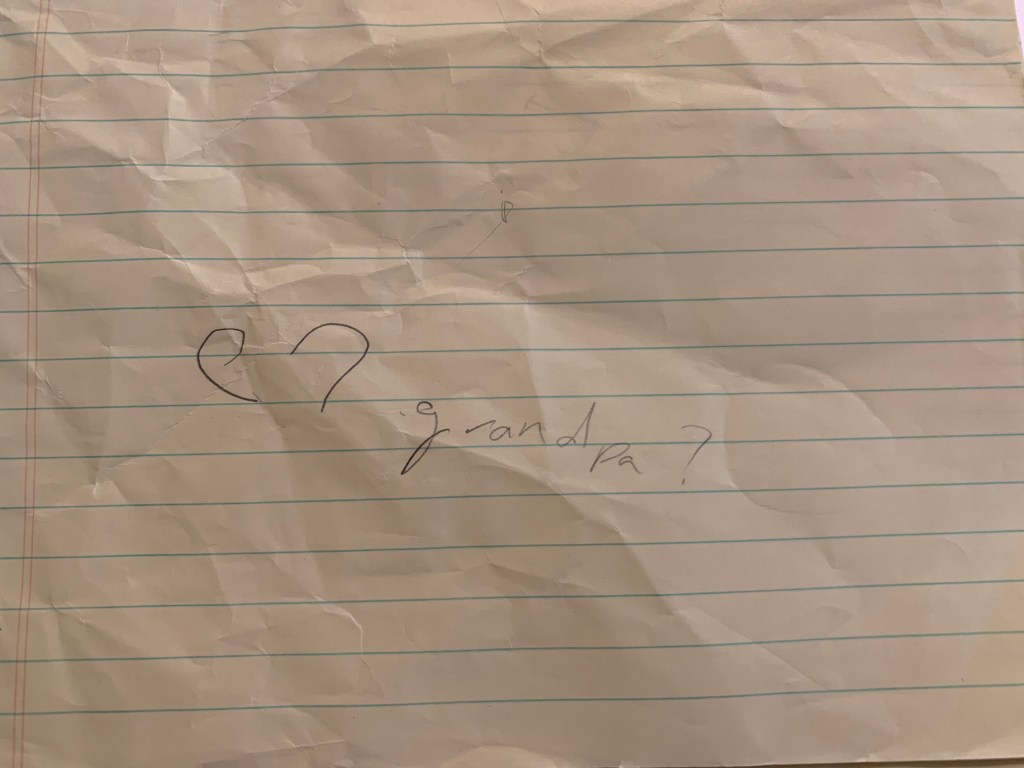
He turned the paper around so we could read it.
“Grandpa?”
When we realized the meaning, she began fighting back tears.
Even completely drugged, a tube down his throat, hands restrained, and in immense pain, he still thought about someone else.
It just blows me away.
MONDAY
I woke up this morning to a text message informing me the doctors were changing his antibiotic.
It felt like a step backwards, but his rash wasn’t improving and thankfully the penicillin did its job fighting off the worst of the infection.
I got moving and readied Sprite and myself.
As we ate breakfast, I received another text message that his breathing was removed.
I REALLY wanted to be present for this momentous, and much desired occasion.
But, that’s okay.
His dad was able to be present, and I was ecstatic the tube was finally removed.
I finally made it to the hospital and saw him de-tubed.
Although he was hoarse, it was a step back to normal.
I was also informed the surgeon already cleared him for no surgery!
The relief was visible.
The remainder of the morning was uneventful, which was quite the shift and wonderfully welcomed.
During lunch Brent was given a swallow test and began some physical therapy.
Let me remind you – he was bedridden, on a ventilator for 5 days.
His body was tired, atrophied, healing, and still fighting the infection.
Later when I asked how PT went, he said it was some of the most intense pain he ever felt.
Following this, a handful of nurses arrived with a machine to assist with healing.
They brought something called a Wound Vac.
The Wound Vac is a machine with a sponge-like extension that sit in a large wound and help extract all the infectious fluid.
Yeah, the name of the device is also its descriptor.
It’s a wound vacuum.
The sponges are literally packed into the wound.
The tubing takes the vacuumed fluid and deposits it in a container.
Y’all, the color of the fluid was…special – brown and red.
But, as gross as that was, it was literally removing all of that from his body.
All of that infectious fluid removed speeds up healing.
And, interestingly enough, the sponges are laced with silver, which is a natural anti-microbial metal.
So, even as it sits in there for a day or three, it doesn’t grow bacteria.
As we learned about its dynamic, Brent was doubtful.
But, I can tell you, after watching it for days – what was collected, the look of his wounds (on the outside), and all the other indicators, it definitely works.

1 thought on “Growing Hope”